Connect With Us
Blog

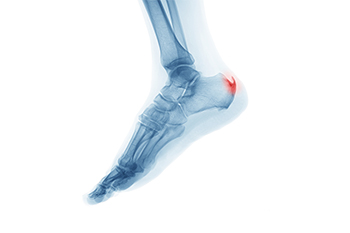
Treating Heel Pain

Heel pain is one of the most common complaints seen in podiatry offices, and it can affect daily movement and quality of life. While plantar fasciitis is a frequent cause, heel pain can also result from bursitis, stress fractures, nerve entrapment, or inflammation of surrounding soft tissue. A step-by-step evaluation begins with identifying the exact location of the pain, when it occurs, and what activities make it worse. Imaging may be used to rule out less obvious causes. Treatment often begins with rest, supportive footwear, and stretching exercises, followed by custom orthotics or targeted exercise if needed. More persistent cases may require injection therapy or additional medical intervention. Addressing heel pain early can help avoid long-term issues. If your heel pain has not improved with basic at-home care or is interfering with your ability to walk, it is suggested that you see a podiatrist for a proper diagnosis and appropriate treatment.
Many people suffer from bouts of heel pain. For more information, contact one of our podiatrists of APEX Foot & Ankle Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our offices located in Fort Myers, Shellpoint, and Naples, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Heel Pain
Heel pain can be difficult to deal with, especially if you do not know what the underlying cause is. If you ignore your heel pain, the pain can magnify and potentially develop into a chronic condition. Depending on the location of your heel pain, you have developed a specific condition.
One condition is plantar fasciitis. Plantar fasciitis is caused by the inflammation of the plantar fascia, or the band of tissue that connects the heel bone to the base of the toes. The pain from this condition is initially mild but can intensify as more steps are taken when you wake up in the morning. To treat this condition, medication will likely be necessary. Plantar fasciitis is often associated with heel spurs; both require rest and special stretching exercises.
There are various options your podiatrist may suggest for heel pain. Treatment options for heel pain typically include non-steroidal anti-inflammatory drugs (NSAIDS), which may reduce swelling and pain. Other options are physical therapy, athletic taping, and orthotics. In severe cases of heel pain, surgery may be required.
Preventing heel pain is possible. If you are looking to prevent heel pain from developing in the future, be sure to wear shoes that fit you properly and do not have worn down heels or soles. Be sure to warm up properly before participating in strenuous activities or sports that place a lot of a stress on the heels. If you are experiencing any form of heel pain, speak with your podiatrist to determine the underlying cause and receive the treatment you need.
Understanding Lisfranc Injuries

Lisfranc injuries result if bones in the midfoot are broken or ligaments that support the midfoot are torn. The midfoot is key to foot stability and arch support. Injuries can result from trauma, such as a fall, car accident, or sports injury, even something as simple as twisting the foot awkwardly. Although rare, Lisfranc injuries are often mistaken for a simple sprain. Symptoms include swelling, bruising on the top and bottom of the foot, pain while standing or walking, and difficulty bearing weight. The foot may appear misaligned or feel unstable. Left untreated, a Lisfranc injury can lead to chronic pain, arthritis, and long-term disability. A podiatrist can diagnose a Lisfranc injury through a physical exam and imaging tests like X-rays, MRI or CT scans. Treatment depends on severity and may include rest, immobilization with a cast or boot, targeted exercises, or surgical repair to realign and stabilize the bones. If you think you may have this condition, it is suggested that you schedule an appointment with a podiatrist for appropriate treatment.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact one of our podiatrists from APEX Foot & Ankle Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our offices located in Fort Myers, Shellpoint, and Naples, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes, Symptoms, and Treatment for a Broken Foot
One out of ten broken bones is reported to be in the feet. When an object crushes, bends, or stretches the bone beyond acceptable ranges, bones break. A break in the foot is either a fracture or a straight break.
The location of any break can tell you how the break happened. Toes, for instance, break typically as a result of something being kicked hard and with great force. Heel breaks almost always are a result of an improper landing from a tall height. Twists or sprains are the other two frequent occurrences. As with all usual breaks, they result from unexpected accident or sudden injury. As with stress fractures, breaks form as a process over time from repeated stress on already present cracks. Runners, dancers, and gymnasts are the usual athletes who receive this type of break. Stress fractures result from incredible pressure on the feet. It is no surprise these athletes bear the majority of reported fractures.
Pain, swelling, bruising, and redness are all indicative of the typical symptoms from a broken foot. Severe pain—to the point of not being able to walk—usually depends on the location of the break in the foot. Toes are on the lower scale of pain threshold, but heels are high, as are a few other particular bones. As the severity of the broken foot increases, symptoms like blueness, numbness, misshaping of the foot, cuts, or deformities will become apparent. These symptoms indicate the need to see a medical professional with access to an x-ray facility.
Prior to seeing a specialist, precautions should be taken to reduce pain and swelling. Elevate and stabilize the foot, and refrain from moving it. Immobilization of the foot is the next priority, so creating a homemade splint is acceptable. Keep in mind that while creating a splint, any increase of pain or cutting off blood circulation means that the splint should be removed immediately. Use ice to decrease swelling and relieve pain symptoms.
When dealing with a medical center, the patient should note that the treatment can vary. The treatment will depend on the severity of the fracture and the cause of the break. Crutches, splits, or casts are common treatments while surgery has been known to be used in more severe cases in order to repair the break in the bones.
What Causes Plantar Fasciitis?

Plantar fasciitis is one of the most common reasons for heel pain, especially in adults who spend a lot of time on their feet. It occurs when the thick band of tissue that runs along the bottom of the foot becomes irritated or strained. Repeated stress from walking, running, or standing for long periods can lead to small tears in the tissue. Wearing unsupportive shoes, having flat feet or high arches, and tight calf muscles can also increase the risk. Pain is usually worse with the first steps in the morning or after sitting for a long time. Left untreated, it can become a long-lasting issue that affects daily movement. If you are feeling sharp or aching pain under your heel, it is suggested you see a podiatrist for a proper diagnosis and appropriate treatment.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from APEX Foot & Ankle Center. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our offices located in Fort Myers, Shellpoint, and Naples, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
What Is a Heel Spur?
A heel spur is a bony growth that develops on the underside of the heel bone, often where the plantar fascia attaches. It typically forms over time as a response to ongoing stress or pressure on the foot. One of the main contributing factors is aging, as the tissues naturally lose elasticity and strength. Abnormal stress from repetitive activities, poor foot function, or walking patterns can place excessive strain on the heel. Carrying extra weight increases the load on the feet, which can lead to small tears in the plantar fascia. These micro-tears trigger inflammation and can encourage calcium deposits to build up, forming a spur. If you have heel pain, it is suggested that you schedule an appointment with a podiatrist who can accurately diagnose and treat heel spurs.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact one of our podiatrists from APEX Foot & Ankle Center. Our doctors will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our offices located in Fort Myers, Shellpoint, and Naples, FL . We offer the latest in diagnostic and treatment technology to meet your needs.
Heel Spurs
Heel spurs are the result of calcium deposits that cause bony protrusions on the underside of the heel. Heel spurs are usually painless, but they have the potential to cause heel pain. Heel spurs tend to be associated with plantar fasciitis, which is a condition that causes inflammation of the band of connective tissue that runs along the bottom of the foot. They most often occur to athletes whose sports involve a lot of running and jumping.
Some risk factors for developing heel spurs include running and jogging on hard surfaces, being obese, wearing poorly fitting shoes, or having walking gait abnormalities.
It is possible to have a heel spur without showing signs of any symptoms. However, if inflammation develops at the point of the spur’s formation, you may have pain while walking or running. In terms of diagnosis, sometimes all a doctor needs to know is that the patient is experiencing a sharp pain localized to the heel to diagnose a heel spur. Other times, an x-ray may be needed to confirm the presence of a heel spur.
Heel spurs can be prevented by wearing well-fitting shoes that have shock-absorbent soles. You should also be sure that you are choosing the right shoe for the activity you want to partake in; for example, do not wear walking shoes when you want to go on a run. Additionally, maintaining a healthy weight can be beneficial toward preventing heel spurs, as it will prevent an excess amount of pressure being placed on the ligaments.
There are a variety of treatment options for people with heel spurs. Some of these include stretching exercises, physical therapy, shoe inserts, or taping and strapping to rest stressed muscles and tendons. If you have heel pain that lasts longer than a month, don’t hesitate to seek help from a podiatrist. Your doctor can help you determine which treatment option is best for you.
Are You Suffering From Ingrown Toenails?
Understanding Neuropathy in the Feet

Neuropathy is a condition that affects the nerves, often causing pain, tingling, numbness, or weakness in the feet. It is commonly linked to diabetes, but can also result from injuries, infections, vitamin deficiencies, or exposure to certain toxins. Over time, damaged nerves can make it difficult to feel sensations or control muscle movement in the feet. Symptoms may begin subtly with a tingling or burning feeling, then progress to sharp pain, numbness, or a pins and needles sensation. Some people may also notice muscle weakness or a loss of balance. These symptoms can interfere with daily activities and increase the risk of foot injuries. A podiatrist can diagnose neuropathy through a physical exam and tests to assess nerve function. Treatment options include medication to manage pain, lifestyle recommendations, targeted exercises, and custom orthotics to support foot health and reduce pressure. Preventing further nerve damage is a key focus. If you have symptoms of this condition, it is suggested that you schedule an appointment to see a podiatrist for a diagnosis and appropriate treatment.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with one of our podiatrists from APEX Foot & Ankle Center. Our doctors will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our offices located in Fort Myers, Shellpoint, and Naples, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blog Archives
- June 2025
- May 2025
- April 2025
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020
- September 2020
- August 2020
- July 2020
- June 2020
- May 2020
- April 2020
- March 2020
- February 2020
- January 2020
- December 2019
- November 2019
- October 2019
- September 2019
- August 2019
- July 2019
- June 2019
- May 2019
- April 2019
- March 2019
- February 2019
- January 2019
- December 2018
- November 2018
- October 2018
- September 2018
- August 2018
- July 2018
- June 2018
- May 2018
- April 2018
- March 2018
- February 2018
- January 2018
- December 2017
- November 2017
- October 2017
- September 2017
- August 2017
- July 2017
- June 2017
- May 2017
- April 2017
- March 2017
- February 2017
- January 2017
- December 2016
- November 2016
- October 2016
- September 2016
- August 2016
- July 2016
- June 2016
- May 2016
- April 2016
- March 2016
- February 2016
- January 2016